Wisdom Teeth
 By the age of 18, the average adult has 32 teeth; 16 teeth on the top and 16 teeth on the bottom. The teeth in the front of the mouth (incisors, canine, and bicuspid teeth) are ideal for grasping and tearing off food into smaller bite size pieces. The back teeth (molar teeth) are used to grind food up into a consistency suitable for swallowing. The last four teeth to erupt are your third molars, also known as “wisdom teeth.” While most other teeth have fully erupted by age 12, this is the time when the wisdom teeth are starting to calcify and form. The average mouth usually has enough room to hold only 28 teeth. When the third molars do not have enough room to erupt, they can form in various different angulations, also known as being impacted.
By the age of 18, the average adult has 32 teeth; 16 teeth on the top and 16 teeth on the bottom. The teeth in the front of the mouth (incisors, canine, and bicuspid teeth) are ideal for grasping and tearing off food into smaller bite size pieces. The back teeth (molar teeth) are used to grind food up into a consistency suitable for swallowing. The last four teeth to erupt are your third molars, also known as “wisdom teeth.” While most other teeth have fully erupted by age 12, this is the time when the wisdom teeth are starting to calcify and form. The average mouth usually has enough room to hold only 28 teeth. When the third molars do not have enough room to erupt, they can form in various different angulations, also known as being impacted.
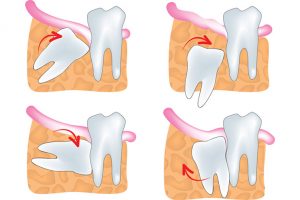
There are many different forms of impaction, whether vertical or horizontal. The extraction of wisdom teeth is necessary when they are prevented from properly erupting within the mouth. They may grow sideways, partially emerge from the gum, and even remain trapped beneath the gum and bone. Impacted teeth can take many positions in the bone as they attempt to find a pathway that will allow them to successfully erupt. Many times, wisdom teeth are accessory teeth and have inadequate root morphology to function as regular molars. Even when they align properly and fully erupt, they are very difficult to maintain proper hygiene and at a high risk of problems in the future.
Indications for Wisdom tooth removal
Wisdom teeth may need to be extracted due to infection and pain. Impacted teeth can be partially erupted, causing a deep opening around the teeth that allows bacteria to grow and become infected. The flap of tissue that covers the partially submerged wisdom tooth (called the operculum) creates a deep pocket that cannot be properly cleansed even with proper brushing and flossing. As debris and bacteria accumulate, one can experience cycles of pain and pressure due to inflammation and infection. This condition is called pericoronitis. Once the offending tooth is removed, the deep pocket will disappear along with the symptoms.
Even when fully erupted, the teeth are difficult to properly maintain due to limited access. Therefore, they are much more prone to cavities. Once a cavity develops in a wisdom tooth, extraction is usually recommended because the access is very poor and restoration with fillings and crowns can be difficult.
Cyst formation and pathology
As the wisdom tooth forms, a group of cells that created the tooth buds, called the follicle, remains around the crown of the tooth. When impacted and untreated over long periods of time, the cells within the follicle can cause formation of a tumor or cyst. A cyst is a fluid filled sac lined with follicular cells. They are usually not cancerous and cannot spread to other parts of the body; however, when untreated, they can grow to very large sizes to cause local destruction of the jawbone and adjacent teeth. When your surgeon removes your wisdom teeth, he also removes the follicular sac to prevent formation of such cysts.
Long term health of adjacent teeth
Growth of teeth roots and cysts can displace and resorb bone as it forms. When wisdom teeth are removed, a variable amount of bone will need to be removed as a standard technique of the surgery, depending on the degree of impaction. When wisdom teeth are removed at a young age (i.e. mid-teenage years), 90 – 100% of the bone will grow back. However, when they are removed at a later age, only a fraction of the bone will regenerate. This results in a persistent pocket or bony defect behind the second molars that can become problematic. It emphasizes the need to have wisdom teeth treated early to prevent this and many other potential complications.
Movement of orthodontically corrected teeth
Some dentists and orthodontists believe that pressure and force from erupting wisdom teeth can cause movement and relapse of orthodontically aligned teeth. This movement happens very slowly over months and years. Removal of the offending wisdom teeth and use of your orthodontic retainers could prevent this potential problem.
Potential nerve damage and lip numbness
Possible damage to the nerves that supply sensation to your lip, chin and tongue are inherent potential complications that can occur with removal of lower molars, especially wisdom teeth. When these teeth are removed early, the root formation is incomplete and not in close proximity to the nerve trunk. Therefore, the possibility for lip and chin numbness is essentially zero. As the roots grow, they can form hooks and loops that can touch or even wrap around the nerve trunk. Subsequently, damage to these nerves during removal is much higher at later ages (i.e. late 20s and older). Rarely, the numbness and tingling can be permanent. Early removal is highly recommended to avoid such future problems and to decrease the surgical risk involved with the procedure.
Anesthesia
In most cases, the removal of wisdom teeth is performed under I.V sedation. Dr. Gill will administer medications through an I.V. to ensure that you do not remember most of the surgery. All outpatient surgery is performed under appropriate anesthesia to maximize patient comfort. Dr. Gill has the training, license and experience to provide various types of anesthesia for patients to select the best alternative. He is a Fellow of the American Society of Dental Anesthesiology and a Diplomate of the National Board of Dental Anesthesiology, a distinction held by a select number in the province.
Teenage years are the usual time periods when dental fears and anxiety can develop due to traumatic and painful experiences. These bad experiences can last a lifetime. Therefore, it is very important that your surgical visit with us is as non-traumatic and as comfortable as possible.
You will rest under our supervision in the office until you are ready to be taken home. Upon discharge, your postoperative kit will include instructions after surgery, a prescription for pain medication, antibiotics, and a follow-up appointment in 1-2 weeks.
Our services are provided in an environment of optimum safety that utilizes modern monitoring equipment and staff who have extensive experience in anesthesia techniques.
Timing
The key to successful and uneventful recovery from wisdom teeth surgery is young age. The later the surgery, the more difficult the recovery. Therefore, one should not wait until the teeth start to hurt, because by then it could be too late. The ideal time for treatment is during the teenage years, i.e. 15 – 18 years old. The recovery becomes significantly more difficult when treated during the late 20’s, 30’s or higher. At age 16, for most patients, fully recovery is less than one week. At age 30 or above, complete recovery could take up to a month. Furthermore, potential complications, such as nerve damage, sinus exposure, infection and jaw fracture are much higher at a later age.
Common Side Effects:
Bleeding
A certain amount of bleeding is to be expected following surgery, and slight oozing, or redness in the saliva is not uncommon. Excessive bleeding may be controlled by placing a gauze pad over the area and biting firmly for 30 minutes. Repeat as often as needed. In the absence of clotting disorders, most bleeding can be controlled with direct pressure. If bleeding continues, you can bite on a moistened tea bag for 30 minutes. The tannic acid in the tea bag helps to form a clot by contracting bleeding vessels. To minimize further bleeding, sit upright, do not become excited, and avoid strenuous exercise.
Stitches are placed in the area of surgery to minimize post-operative bleeding and to help healing.
Unless otherwise stated, these stitches are dissolvable. They will last in the wound between 2-7 days. Dissolution of the sutures within this time period is normal and need not be replaced.
Swelling
Your face and cheeks could be dramatically swollen in the next 48 hours. Your doctor has given you medicines during the surgery that minimizes the swelling, but it cannot be completely eliminated. The swelling that is normally expected is usually proportional to the surgery involved. Swelling around the mouth, cheeks, eyes and sides of the face is not uncommon. This is the body’s normal reaction to surgery and eventual repair. The swelling will not become apparent until the day following surgery and will reach its maximum peak the second day after surgery. However, the swelling may be minimized by the immediate use of ice packs. Two plastic bags filled with ice, or ice packs should be applied to the sides of the face where surgery was performed. The ice packs should be left on for intermittent periods while you are awake for the first 48 hours.
Discoloration
In some cases, Bruising and skin discolorations follows swelling and are not unusual. The discolorations can be yellow or black and blue, depending on the fairness of your skin, and is usually limited to the neck or cheek area near the surgical site. This is caused by blood spreading beneath the tissues and through the mucous membranes in the mouth. This is a normal postoperative occurrence, which may occur two to three days after the procedure. It is temporary, but often takes upto a week for this to completely disappear.
Pain
As with all surgery, there will be varying degrees of pain and discomfort following the procedure. To provide baseline pain relief, extra strength Ibuprofen (Advil) will be prescribed every six hours. This tablet is equivalent to three over the counter Advil or Ibuprofen tablets. Therefore, YOU CANNOT TAKE MORE THAN FOUR TABLETS PER DAY. One tablet every six hours will provide adequate pain relief for most situations with minimal side effects. Additionally, it will minimize swelling and decrease the requirements of the stronger narcotic analgesics (i.e. Tylenol #3 or similar)
If the pain relief is inadequate from the ibuprofen, an additional narcotic medication for breakthrough pain will be prescribed, Tylenol #3 or similar. Since they are extremely strong and potentially dangerous medicines, they should be used with care. Potential side effects are:
- Nausea and vomiting. WHEN TAKEN ON AN EMPTY STOMACH, THEY WILL CAUSE NAUSEA, therefore, be sure to take the medicine with food or thick liquids.
- Constipation. If you are prone to constipation, pre-emptive laxatives or prune juice when taking these medicines is advised.
- Decreased mental capacity. They will also make you groggy and will slow down your reflexes, so do not drive an automobile or work around machinery. Avoid alcoholic beverages.
- Addiction and dependence. Prolonged use and abuse of these medications can lead to drug dependence and addiction. If the discomfort is manageable with the prescription strength Ibuprofen, please refrain from taking these medicines as much as possible.
Pain or discomfort following surgery should subside more and more each day. If pain persists, it may require attention and you should call the office.
There will be a period of discomfort associated with the surgery. Please remember that everyone tolerates pain differently. One person could take one week to heal for the same procedure that another person could recover in two days.
Nausea & Vomiting
Nausea and vomiting is a common side effect of the anesthesia and the narcotic pain medicine. In the event of nausea and/or vomiting following surgery, you should not take anything by mouth for at least an hour including the prescribed medicine. You should then sip on a warm, clear broth-based soup, hot tea, ginger ale or fruit juice. You should sip slowly over a 15-minute period. Do not take the narcotic pain medication, i.e. Tylenol #3, Percocet, etc., for at least four hours, as these medicines are the likely culprit for your symptoms. In most cases, the Ibuprofen should not cause nausea by itself.
Numbness and tingling of lower lip, chin and tongue.
Numbness of the tongue, lower lip and chin is a potential complication of extracting lower wisdom teeth. You should be aware that immediately after surgery your lip or tongue will be numb from the “Novocaine”. Thus, you could bite it and not feel the sensation – so be careful. These symptoms should disappear by the next day. If you continue to experience the numbness and tingling for two days after surgery, please contact our office. The injury is usually temporary, but full recovery can take up to six months.
Infection
If you have continuing pain, swelling, fever and a bad taste in your mouth after a week following surgery, it is possible that you have an infection at the extraction sites. If you experience these symptoms a week after the surgery, please contact our office for a visit.
With all surgeries, the potential for infection is always present, but rare (< 10%). Antibiotics will not be prescribed for routine surgical procedures unless there are extenuating circumstances. It is our belief that indiscriminate and irresponsible use of antibiotics is not beneficial and potentially much more harmful due to inherent side effects and future bacterial resistance to infection. However, for exceptionally difficult cases or other comorbid medical conditions, your doctor might choose to prescribe a short course of antibiotics to help prevent an infection. Please make sure you take the tablets or liquid as directed. We advise that you discontinue antibiotics in the event of a rash or other unfavorable reaction and notify our office. If you were prescribed an antibiotic and are currently taking oral contraceptives, you should use an alternate method of birth control for the remainder of this cycle.
A slight elevation of temperature immediately following surgery is not uncommon. If the fever occurs within 24 hours after the surgery, it is usually not an infection, but rather a normal side effect of the anesthesia. The effect is temporary and should subside.
Joint pain, stiffness and limited opening
Stiffness (trismus) of the jaw muscles may cause difficulty in opening your mouth for a few days following surgery. This is a normal post-operative event and physiological response to surgical trauma that will resolve slowly over a couple of weeks.
Dry Socket
A dry socket is a condition in which the blood clot that has formed in the extraction socket has either dislodged or dissolved prematurely from the tooth socket. It is a very painful condition along the surgical site occurring five to seven days following surgery, often radiating toward the ear and forward along the jaw which may cause other teeth to ache. Fortunately, it is a self-limiting process and with adequate pain control, resolves itself in 24 – 48 hours. It is up to ten times more common in smokers.
Occasionally, you may feel hard projections in the mouth with their tongue. They are not roots; they are the bony walls, which supported the tooth. These projections usually smooth out spontaneously. To speed the healing process, do not touch the area with your tongue and limit chewing to the opposite side.
There will be a large void where the tooth was removed. This void will gradually fill in with new tissue over the next month. In the meantime, the area should be kept clean especially after meals with salt-water rinses or a toothbrush, starting 3 days after surgery. A curved syringe will be given at the follow up visit to help keep the sockets free of debris.
Sinus exposure
Your upper wisdom teeth and molars are close to the sinus, which are two air-filled cavities above your upper teeth and behind your cheekbones. The sinus becomes larger over time and could surround the roots of the teeth. When the teeth are removed, it is possible to have an exposure into the sinus at the extraction site. In the majority of cases, these exposures close spontaneously, but precautions should be taken during the healing period.
Potential long-term complications
Fortunately, the chance of these complications occurring is extremely rare. For extremely difficult cases, your doctor will inform you if there is an above average chance of these complications occurring.
- Permanent lip, chin and tongue numbness
- Jaw fracture
Please remember…
Dr. Gill has performed thousands of this exact type of surgery and has extensive experience in the procedure. However, healing and recovery is extremely variable with every individual and cannot be controlled. Your case is unique and no two mouths are alike. Do not accept well-intended advice from friends and family, as their experience might be drastically different from yours.
